Table of Contents
Q What are Heberden's Nodes?
A common condition affecting the distal interphalangeal joints (DIP joints), known as "Heberden's nodes," is characterized by the formation of two bony nodules on the dorsal side of the first joint.

Inflammation of the joint leads to the loosening of the joint capsule, causing the joint to bend in a flexed direction (resulting in an inability to fully extend the DIP joint). Additionally, worn-down bone can stimulate the growth of irregular bone formations around the joint, leading to bony protrusions known as osteophytes. This condition often affects multiple fingers rather than a single one and is most commonly observed in women over the age of 40.
Cause of Heberden’s nodes
The exact cause of Heberden's nodes is unknown.
However, due to its characteristics, it is considered a type of osteoarthritis, suggesting that aging and overuse are contributing factors. It is particularly common in women over 40 and individuals who are obese, indicating that lifestyle factors, such as diet, may also play a role.
Additionally, frequent and strenuous use of the hands is thought to be a contributing factor. This condition is often observed in individuals engaged in occupations like farming and other manual labor.
Symptoms of Heberden’s nodes
Symptoms such as redness, swelling, pain, and a persistent bent position can appear in the DIP joints from the index finger to the little finger.
The range of motion in the DIP joints becomes restricted, leading to impaired movement. Pain may make it difficult to grip objects firmly. Individuals may experience pain during finger movements or even at rest. Activities like washing dishes, typing on a computer, or holding chopsticks can become challenging. In rare cases, symptoms may also appear in the thumb.
How is Heberden’s nodes diagnosed?
The diagnosis of Heberden's nodes is based on swelling (edema) of the DIP joints and characteristic findings on X-rays, such as joint space narrowing and bony protrusions.
Other conditions to consider include rheumatoid arthritis, psoriatic arthritis, and gout. Since each of these diseases has distinct features, it is advisable to undergo testing at a specialized medical facility for an accurate diagnosis.
Prevalence of Heberden's Nodes
According to previous reports**, Heberden's nodes and joint deformities are not uncommon, with 10.6% of individuals in their 30s being affected. The prevalence increases with age:
- 30s: 10.6%
- 40s: 20.7%
- 50s: 28.6%
- 60s: 35.3%
- 70s: 50.5%
- 80s: 59.1%
** K Fujisawa et al: Heberden’s node- Morbidity survey in the general population - Jpn. Soc. Surg. Hand, 4:769-772, 1987.
Preventive Measures for Heberden's Nodes
Heberden's nodes are caused by the progressive wear and tear of joints, and there is currently no established method to halt their progression. However, the following measures can help in prevention:
Joint Protection
- Use splints or other supports to minimize strain on finger joints.
- Avoid tasks that place excessive pressure on the joints.
- Avoid applying pressure in the opposite direction to prevent deformity
- Avoid vigorous or excessive massaging of the joint
Recommended Food
- Soy Products: Foods made with soy milk and other soy-based products are highly recommended.
- Anti-inflammatory Foods: Consuming foods rich in DHA and EPA, omega-3 fatty acids known for their anti-inflammatory properties, is beneficial. Examples include mackerel, sardines, and other oily fish.
Foods to Avoid
- High-Calorie and High-Sugar Foods: Excessive consumption of sweets and high-sugar diets can lead to inflammation around the joints. Reducing carbohydrate and sugar intake is advised. For those who haven’t monitored their carbohydrate consumption, cutting portions of rice, bread, pasta, and sweets in half can be a good starting point.
- Caffeine: Some studies suggest a possible link between caffeine consumption and the development of Heberden's nodes. If concerned, consider reducing caffeine intake or switching to decaffeinated or low-caffeine beverages.
- Alcohol: Avoid alcohol, as it dilates blood vessels throughout the body. In Heberden's nodes, abnormal blood vessel growth around the joints often leads to pain when accompanied by nerve involvement. Alcohol consumption can intensify the throbbing pain commonly reported by patients.
By incorporating these measures into your lifestyle, you can help reduce the risk of developing Heberden's nodes and minimize stress on your joints.
Progression of Heberden's Nodes
Heberden's nodes typically progress over a period of around 10 years if left untreated, with deformity gradually worsening. It is common for symptoms to spread to other fingers over time.
- Early Stages: Symptoms typically begin with swelling, redness of the skin, and joint pain.
- Intermediate Progression: Over several years, the affected joints may become increasingly deformed.
- Advanced Stages: The joints eventually stabilize in a fixed position, either bending sideways (lateral deviation) or becoming flexed. At this stage, pain often subsides, but the deformity becomes permanent.
To prevent progression, it is advisable to address inflammation during the early stages of pain. While treatments like steroid injections provide temporary relief, there was previously no definitive cure. However, a new treatment method involving intra-arterial therapy, which takes just five minutes, has recently become available. Consider exploring this option for effective management.
Mucous Cyst in Heberden's Nodes
A mucous cyst is a condition often associated with Heberden's nodes. It occurs when joint fluid from the distal interphalangeal (DIP) joint bulges outward due to joint deformity. These cysts are small, fluid-filled sacs that form near the first joint of the finger.

Key Features:
- Appearance: A small, translucent or semi-translucent bump near the fingertip joint.
- Connection to the Joint Capsule: The cyst is directly linked to the joint, allowing joint fluid to leak into the cyst.
- Potential Complications: If popped or punctured, the cyst can become infected due to bacteria entering through the skin.
Precautions:
It is crucial not to attempt to pop or manipulate the cyst yourself, as this may lead to infection. Seek medical advice if the cyst becomes painful or grows larger.
Treatment Options for Heberden’s Nodes
The treatment options for Heberden's nodes generally include well-known conservative therapies such as rest or taping and a newly developed method called Arterial Injection Treatment.
Conservative treatment:
This treatment focuses on relieving pain and inflammation while minimizing the impact on daily life.
- Painkillers (NSAIDs): Medications such as loxoprofen or ibuprofen may be prescribed to reduce inflammation and pain.
- Topical Medications (Patches & Creams): Anti-inflammatory patches or creams can help relieve pain.
- Taping & Orthotic Therapy: Taping or using orthotic devices helps stabilize the joint and limit excessive movement.
- Heat Therapy: Applying heat improves blood circulation and alleviates pain.
Steroid Injections
If the inflammation is severe, steroid injections may be administered into or around the affected joint to temporarily reduce pain and swelling.
However, long-term use should be approached with caution, as it may cause side effects such as cartilage damage.
Consultation
Recently, it has been discovered that osteoarthritic joints often develop excess blood vessels, which contribute to swelling, inflammation, and pain. A new treatment designed to reduce these blood vessels has been developed. This procedure is simple, taking only about five to ten minutes, and has shown better results than traditional treatments.
Although joints that have already deformed cannot be restored to their original state, starting treatment early (within the first few years of inflammation) can halt the progression of deformity.
For more information about our newly introduced Arterial Injection Treatment, please refer to the following link:
Author

-
I began my career as an interventional radiologist, which led to my research on pathological angiogenesis during graduate school. As first author, I published findings on related genes in Nature Medicine in 2012. Based on this work, I developed a novel embolization treatment for chronic musculoskeletal disorders, such as knee osteoarthritis and frozen shoulder, and was the first to report its safety and effectiveness. This approach is now being studied internationally.
-Career-
2006-2009 Fellow, Department of Radiology, Clinica ET, Yokohama, Japan
2009-2012 Researcher, Center for Integrated Medical Research, Keio University, Tokyo, Japan
2012-2015 Clinical Researcher, Department of interventional radiology, Edogawa Hospital, Tokyo, Japan
2015-2017 Director, Musculoskeletal Intervention Center, Edogawa Hospital, Tokyo, Japan
2017- Chief Director, Okuno Clinic., Tokyo, Japan
Latest posts
 Sep 12, 2025Gout FAQ
Sep 12, 2025Gout FAQ May 30, 2025Heberdens Nodes FAQ
May 30, 2025Heberdens Nodes FAQ Dec 27, 2024Prostatitis FAQ
Dec 27, 2024Prostatitis FAQ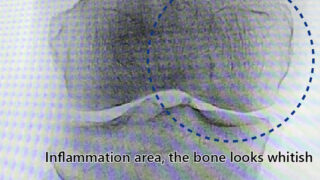 Dec 27, 2024Knee Osteoarthritis FAQ
Dec 27, 2024Knee Osteoarthritis FAQ