Table of Contents
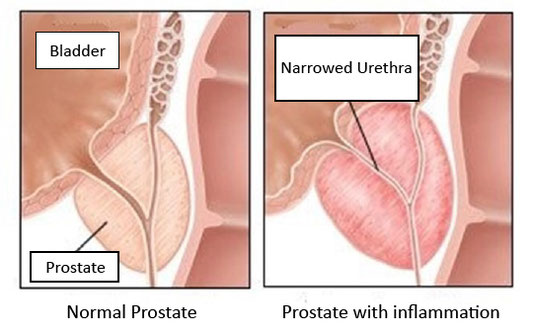
Q What is Prostatitis?
Prostatitis is a disease that causes swelling and inflammation of the prostate gland, resulting in difficult urination and pain. The prostate gland is just below the bladder and has functions for nourishing sperm, regulating pH, and transporting sperm. It is most common in men between the ages of 35 and 50, but can affect teenagers or men in their twenties and is experienced by 10% to 15% of men.
What is the cause of Prostatitis?
There are two types of Prostatitis: acute prostatitis and chronic prostatitis, that lasts more than three months. Most acute cases are caused by bacterial infection, whereas only 10% of chronic prostatitis cases can be attributed to such an infection. Most cases are chronic prostatitis which are not related to bacterial infection, with the cause never identified.
Bacterial prostatitis is caused by retrograde infection from the urinary tract (bacteria enter through the urethra and travel in the opposite direction of urine). Treatment with antibiotics is effective but can cause continual recurrence if not properly treated.
The cause of prostatitis not related to bacterial infection, is not yet known in detail. There are various hypotheses for its occurrence, for example that prostatitis an autoimmune reaction to the prostate gland, or that the prostate gland is inflamed by the contents of urine, or that the surrounding nerves and muscles are dysfunctional.
Risk factors for prostatitis:
You are more likely to have prostatitis if these factors apply to you:
- Young or middle-aged people
- Prostatitis in the past
- Urethritis or cystitis in the past
- Pelvic injuries due to biking, horseback riding, etc.
- Previous urethral catheterization
- Previous prostate biopsy
What are the symptoms of Prostatitis?
Symptoms of prostatitis include:
- Frequent urination, urinary urgency (need to urinate immediately)
- Frequent urination at night
- Strong pain when urinating
- Difficulty in urinating, especially at the onset of urination
- Back pain
- Constipation
- Lower abdominal pain
- Pain or numbness at the base of the leg or thigh
- Blood in urine
- Sensation of residual urine
- Pain during erection
- Discomfort
- Pain in the area between the testicles and anus
- In addition to the above symptoms, prostatitis caused by bacterial infection can cause flu-like symptoms such as feeling chilly and fever.
Prostatitis Diagnosis
The following is the diagnosis procedure for prostatitis:
- You will be asked about your history and symptoms during a medical consultation. In addition, the following tests will be performed to differentiate prostatitis from other diseases and to diagnose the type of prostatitis.
- Urinalysis
If prostatitis due to bacterial infection is suspected, a urinalysis will be performed to confirm the presence of pyuria or bacteriuria. - Blood test
Inflammation markers will be checked to determine whether the disease is acute or chronic. A tumor marker called PSA is also measured. PSA is also elevated in prostatitis, but it decreases with treatment, so it can be distinguished from prostate cancer. - Rectal Examination
If necessary, a rectal examination is performed. Rectal examination is a manual examination in which the doctor puts on gloves, inserts his fingers into the rectum, and compresses the prostate from the rectal side to see if it is swollen and if the compression causes pain or discomfort. - Imaging Examination
MRI, ultrasound, and CT scans may be performed as imaging tests.
An MRI scan provides an overall view of the pelvic area. It can also detect signal changes due to prostate cancer or inflammation in the prostate.
By performing the above tests, we can divide the patient into the following four types:- Acute bacterial prostatitis
Developing suddenly with cold-like symptoms, it is characterized by fever, chills, nausea, and vomiting. - Chronic bacterial prostatitis
When the bacteria that caused prostatitis are not adequately treated with antibiotics, the infection may recur or become intractable (not responsive to treatment). If the disease becomes chronic, there may be periods of strong symptoms, while others may be asymptomatic or cause only mild symptoms. - Chronic prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
This type of prostatitis which is chronic and occurs without bacterial infection, is the most common of all prostatitis. Here, the cause cannot be identified. Symptoms often persist with equal intensity over a long period of time. In some cases the symptoms come and go repeatedly. - Asymptomatic inflammatory prostatitis
This type does not have any symptoms and is found by the presence of white blood cells in a urine test by chance. It does not require any specific treatment.
- Acute bacterial prostatitis
Prostatitis Treatment
The first treatment prescribed for prostatitis is 500 mg of fluoroquinolone antibiotic (product name: Cravit **may vary depending on country), taken once daily for 2-4 weeks or 6 weeks at longest. This treatment is effective enough for acute bacterial prostatitis, and even for chronic prostatitis with around half of chronic prostatitis patients reporting improvement in their symptoms.
However, chronic prostatitis may not improve with antibiotics, and a combination of several medications may be needed, depending on the symptoms:
- Harnal may be prescribed as a muscle relaxer to improve urinary tract symptoms such as frequent urination.
- Non-steroidal anti-inflammatory drugs such as Loxonin,
- A pain reliever called Tramal
- Anti-anxiety medication such as Depas.
- Myonal, a muscle relaxant, may also be prescribed to reduce muscle overstrain.
- Cymbalta, an antidepressant, is also sometimes prescribed.
- A plant-derived medicine called Cernilton to reduce inflammation of the prostate gland. It is made from an extract of a Western-developed plant pollen mixture (thymus, corn, rye, hazel, pussy willow, boxelder, frangipani, and pine) and is taken two tablets two to three times a day.
In addition to the above oral treatment, lifestyle modification, stretching of pelvic floor muscles, physiotherapy therapy, psychotherapy, and prostate massage. Surgery is also available but is less common.
Recently, a new treatment method called catheterization is available to reduce the number of problem blood vessels created by the inflammation.
Q Are there any herbal medicines that are effective for prostatitis?
A: There are several Chinese herbal medicines that have been reported to be effective in the treatment of prostatitis, including Gentian Liver-Purging Decoction(竜胆潟肝湯), Lotus Seed Combination(清心蓮子飲), Bupleurum & Hoelen Combination (柴苓湯) and Cinnamon Twig and Poria Pill(桂枝茯苓丸). For more information, please visit a specialized medical institution.
Q Are there any good over-the-counter medicines for prostatitis?
A: The basic treatment for prostatitis is antibiotics, but most over-the-counter medications are made from herbal preparations or herbal medicine ingredients. No antibiotic or antibacterial preparations are available. Therefore, to improve prostatitis with over-the-counter drugs, the symptoms are suppressed with herbal or herbal medicine ingredients.
Specifically, over-the-counter Chinese herbal preparations available include Gosha-jinki-gan (牛車腎気丸), Gentian Liver-Purging Decoction(竜胆潟肝湯), Rehmannia Eight Formula(八味地黄丸), Ulinar b based on Lotus Seed Combination(清心蓮子飲), and Urination pain medicine called Bokoren in Japanese.
Q What are some ways to treat prostatitis other than taking medications?
A: The first step is diet. Dietary therapy includes avoiding food with a lot of spices, citrus fruits to reduce the irritation of urine passing through the urethra.
Psychotherapy has also been reported to be effective, as stress and psychological factors can also amplify pain and discomfort. Psychotherapy includes reducing daily stress such as through counseling as well as cognitive behavioral therapy.
In addition, improvement of pelvic floor muscle function may also be effective. Surgery is also used in some situations but is not very common. Transcatheter embolization has recently been developed to improve prostatitis.
Q How long does it take to treat prostatitis?
A: Acute prostatitis caused by a bacterial infection generally requires 2-4 weeks of oral antibiotic medication, 6 weeks in the long case.
Also even with chronic prostatitis, it is reported that approximately half people have experienced of improvement or disappearance of symptoms after 6 weeks of Cravit therapy. On the other hand, there are many cases in which the above treatment does not improve. In these cases, it is very difficult to predict or estimate the duration of the treatment. This is because the treatment is symptomatic, and it takes time to reach a level of improvement that does not interfere with daily life.
Q What is the difference between acute and chronic prostatitis?
A: Acute prostatitis has an obvious bacterial infection and develops rapidly. It is characterized by symptoms similar to those seen with influenza, such as fever, feeling chilly and vomiting in addition to prostate symptoms.
If there is an intense bacterial infection of the prostate that does not respond to oral medications, intravenous antibiotics may be used.
Chronic prostatitis lasts for more than three months and its mostly unrelated to bacterial infection and is called Chronic Prostatitis/ Chronic Pelvic Pain Syndrome (CP/CPPS).
Q I have prostatitis. Is there any problem with sexual activity during treatment? Is it safe to ejaculate?
A: If there are no bacteria present, sexual activity is not a problem. In the case of prostatitis caused by chlamydia infection, it is necessary to make sure that the chlamydia has disappeared with treatment. Also, in both cases, masturbation is not a problem.
Q I suffer from chronic sleep deprivation and constipation due to public pain caused by prostatitis. Is there any way to reduce the pain?
A: Pubic pain tends to be prolonged in case of prostatitis. You can relieve the pain in several ways:
First, you can review your lifestyle. Since sitting at a desk for long periods of time puts a strain on the prostate gland. Try to avoid sitting for long periods of time by getting up from your seat every 30 minutes to an hour. Also, avoid using a bicycle, especially one with a seat that digs into your hips, such as a road bike. It is recommended to avoid using bicycles as much as possible. Drinking alcohol and smoking are known to increase inflammation of the prostate gland and they should be avoided.
If the MRI shows evidence of inflammation in the prostate, catheterization as described in our website is recommended.
Q I thought my prostatitis was cured, but it came back. Will there ever be a cure?
A: In treating prostatitis, there is a possibility of recurrence. First of all, if you did not take antibiotics for a long enough period of time during the initial treatment, you should resume taking them. If there is still no improvement, we will address the problem with the other treatments listed above and lifestyle modifications.
Things to avoid with chronic prostatitis
The following should be avoided as they may cause or aggravate prostatitis:
Physical pressure
Since the prostate gland is located deep between the penis and anus, working at a desk or driving for long periods of time (especially bicycling) can cause prolonged pressure on the prostate gland as well. You can lighten the load on the prostate by taking breaks or taking time to stand up once an hour when working at a desk or driving for long periods of time.
If you cannot take a break, you should find and use a cushion that suits you, such as a cushion with an open center, as this may reduce the pressure on the prostate.
Special Sexual Practices
Some sexual acts and sexual services place physical or functional strain on the prostate gland. Repeated stimulation of the prostate through the anus or stopping just before ejaculation can put physical or functional stress on the prostate. This can cause or aggravate prostatitis, so you must be very careful. Also, many people develop bacterial prostatitis triggered by a sexually transmitted infection, which then becomes chronic. Please be as careful as possible.
Excessive alcohol consumption, eating or drinking excessive salt or stimulants
Excessive alcohol consumption, salt, and stimulants such as pepper, horseradish, and hot pepper can cause swelling of the prostate gland, decrease contraction of the bladder, and stimulate inflammation. Try not to take these.
Long-term prostatitis and further diagnosis
When prostatitis becomes chronic, for example for more than one or two years, the sensitivity spreads to other organs in the pelvic region, such as the testicles, anus, bladder, sacral region, lumbar region, and sciatic nerve. This may result in constipation, back pain, and numbness in limbs.
This is common for people with pelvic pain, including bladder and anal pain, as well as for prostatitis, but when people often experience prolonged discomfort or pain in one area, it can cause pain and sensitivity to spill over into the surrounding areas. Fundamentally, curing prostatitis often improves the surrounding symptoms that were spilling over.
If you experience prostatitis for more than a year, and you are concerned, you should seek a professional medical advisor. Usually, other diseases are ruled out when diagnosing prostatitis.
Conditions that present with similar symptoms to prostatitis include the following:
- Prostate cancer: In this case, urethral symptoms like difficulty urinating or increased frequency and sexual pain are common. Blood tests and MRI can give further information.
- Bladder stones: These cause similar symptoms and lower abdominal pain during urination. Diagnosis is made by ultrasound or CT to confirm the presence or absence of stones.
- Musculoskeletal conditions: such as low back pain, hip pain, and pubic symphysis.
Exercises to help prevent prostatitis
Squats
In prostatitis, the pelvic floor muscles are thought to be in a state of hypertonia, where muscle output (exertion of force) is not working properly. Squatting is an effective way to improve the condition of the pelvic floor muscles. It is a moderate full-body exercise and relaxes the overstretched pelvic floor muscle groups.
Please follow the below procedures.
Stand with your feet shoulder-width apart. Your toes and knees should be facing in the same direction.
Slowly bend knees. Imagine there is a chair behind you and bend your knees as if you were sitting on the chair. Once your hips are as low as your knees, slowly extend your hip and knee joints.

Stand with your feet shoulder-width apart.
Your toes and knees should be facing in the same direction.
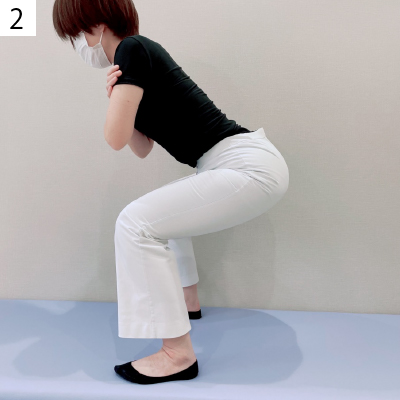
Slowly bend your knees.
Imagine there is a chair behind you and bend your knees as if you were sitting on the chair.
Bad examples of squats

Make sure that your kneecaps do not turn outward.

Make sure that your kneecaps do not turn inward.
Stretches
To loosen the overstretched pelvic floor muscles, it is a good idea to stretch the abdominal muscles and hip adductor muscles which are connected to the pelvis floor muscles.
Stretching the abdominal muscles
Lie on your stomach.
Keeping your pelvis on the floor, bend your upper body back. Your abdominal muscles will be stretched. Keep the posture for 15 seconds. Do this 3-5 times a day.
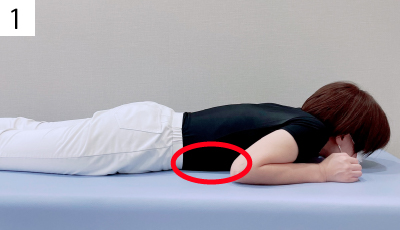
Lie on your stomach
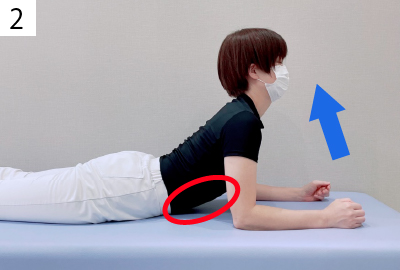
Keeping your pelvis on the floor, bend your upper body back.
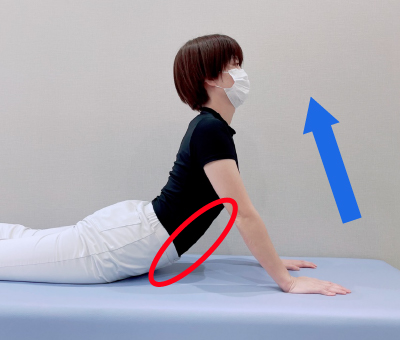
Use your hand to support your body for a better stretch.
Stop if you feel any pain.
Stretching the hip adductor muscles (inner thigh muscles)
Sit on the floor. Place both soles together and open your hip joints.
From this position, lean your body forward. Be careful not to round your back.
Keep the posture for 15 seconds.
This will stretch the inner thigh muscles. Do these 3 to 5 times a day.
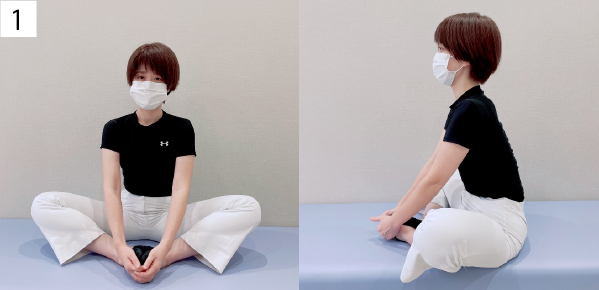
Place both soles together and open your hip joints.

Lean your body forward
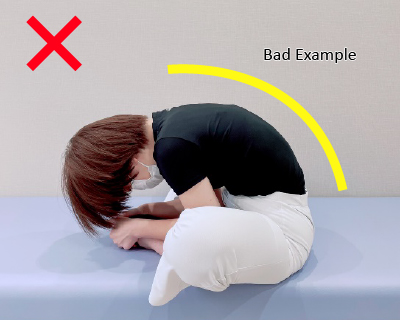
Be careful not to round your back.
Prostatitis and Stress
The pain and discomfort experienced with prostatitis can be exacerbated by stress. This is because stress interferes with the brain’s ability to ‘filter out’ lower priority pain and discomfort signals which come from everyday life. When stress increases, the levels of serotonin and noradrenaline secreted by the brainstem are lower and pain signals are amplified and felt more intensely.
Consultation
Prostatitis is a condition characterized by swelling of the prostate gland. It affects 10-15% of men and results in difficulty urinating and pain. Treatment consists mainly of antibiotics and treating the symptoms. Symptoms often improve following treatment. If you are experiencing any of these symptoms, it is important to see a healthcare professional who can diagnose and treat your condition.
Author

-
I began my career as an interventional radiologist, which led to my research on pathological angiogenesis during graduate school. As first author, I published findings on related genes in Nature Medicine in 2012. Based on this work, I developed a novel embolization treatment for chronic musculoskeletal disorders, such as knee osteoarthritis and frozen shoulder, and was the first to report its safety and effectiveness. This approach is now being studied internationally.
-Career-
2006-2009 Fellow, Department of Radiology, Clinica ET, Yokohama, Japan
2009-2012 Researcher, Center for Integrated Medical Research, Keio University, Tokyo, Japan
2012-2015 Clinical Researcher, Department of interventional radiology, Edogawa Hospital, Tokyo, Japan
2015-2017 Director, Musculoskeletal Intervention Center, Edogawa Hospital, Tokyo, Japan
2017- Chief Director, Okuno Clinic., Tokyo, Japan
Latest posts
 Jan 21, 2026Golfer’s Elbow
Jan 21, 2026Golfer’s Elbow Sep 12, 2025Gout FAQ
Sep 12, 2025Gout FAQ May 30, 2025Heberdens Nodes FAQ
May 30, 2025Heberdens Nodes FAQ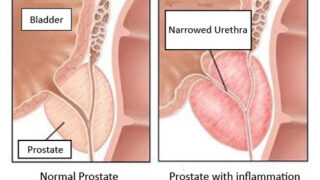 Dec 27, 2024Prostatitis FAQ
Dec 27, 2024Prostatitis FAQ